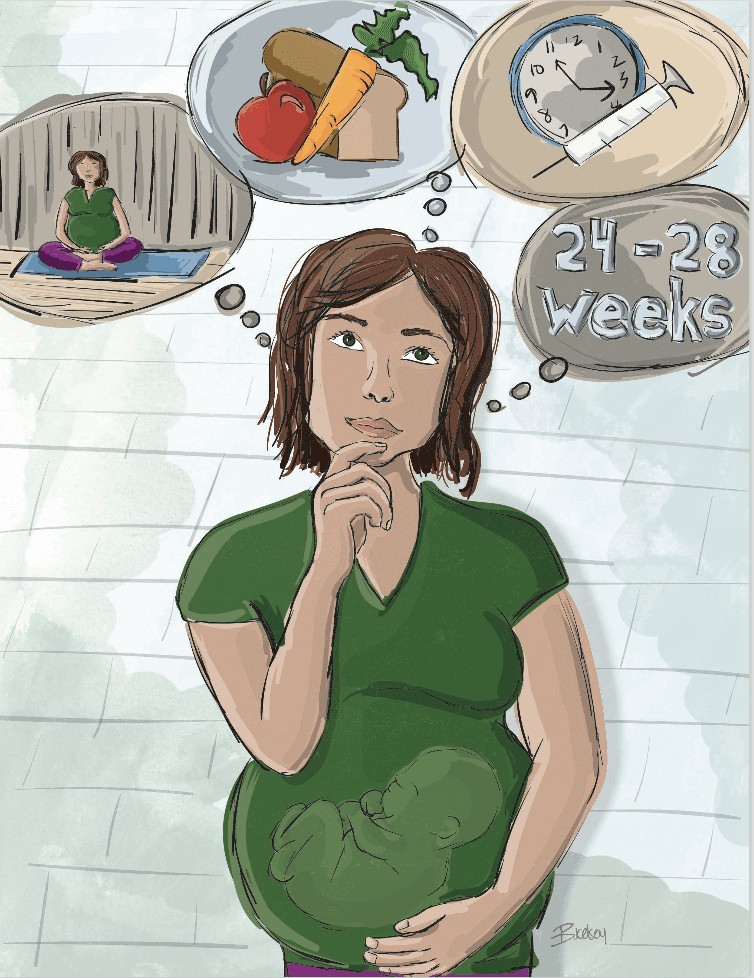
Gestational Diabetes
Based on guidelines from Diabetes Canada. Illustration by Breanne Kelsey.
With a growing risk of gestational diabetes, learn how to stay healthy.
What is gestational diabetes?
A type of diabetes that develops and occurs during pregnancy. Your body cannot produce enough insulin to handle the effort of a growing baby and changing hormone levels, and your blood glucose (sugar) levels rise.
Who develops gestational diabetes?
Up to 20% of pregnant women develop gestational diabetes, however, the women most at risk are those who:
- Are 35 years of age or older
- Are from a high-risk group (Indigenous, Hispanic, South Asian, Asian and African)
- Are obese (body mass index of 30kg/m2 or higher)
- Have prediabetes
- Had gestational diabetes in a previous pregnancy
- Have a parent, brother or sister with Type 2 diabetes
- Have polycystic ovary syndrome (PCOS) or acanthuses nigricans (darkened patches of the skin)
How is gestational diabetes diagnosed?
It is important to be tested for gestational diabetes when you are pregnant, between 24 and 28 weeks gestation, to avoid complications during delivery. Medical laboratories, including DynaLIFE Medical Labs and Calgary Laboratory Services, offer gestational diabetes screenings—you will be given a glucose drink and then a blood sample will be taken. Talk to your physician when you become pregnant to arrange this test and assess your risk.
What happens if I am diagnosed with gestational diabetes?
Gestational diabetes is manageable. You will work with your physician to manage your blood glucose levels through diet, exercise, and insulin to avoid complications in labour and delivery. Your blood glucose levels will return to normal after delivery, however, there is an increased risk of developing Type 2 diabetes permanently and of developing gestational diabetes with future pregnancies. After your pregnancy, it is important to manage your diet and exercise to decrease these risks.
Will my baby be born with diabetes if I have gestational diabetes?
No, but it does increase their risk of developing Type 2 diabetes and becoming overweight. It is important to provide your child with a healthy lifestyle and take preventative measures to decrease the risk of becoming overweight.
Exercise. While you may have to adjust your usual fitness routine, exercise will have a positive impact on your body and can also prevent high blood pressure and chances of post-partum depression. Check with your fitness studio to see if it offers specially prenatal classes or adjustments during regular classes, and work with an instructor who knows how to keep you safe and healthy. Some great options are prenatal classes at Blitz Conditioning in Edmonton, prenatal Pilates at Redefining Eve in Edmonton, prenatal yoga at Junction 9 in Calgary, and barre classes at Barre Body Studio in Edmonton and Calgary (the instructors are pros at adjustments for pregnant women). Talk to your physician about exercise while pregnant to learn what is appropriate for you and your body.
Eat well. Eat smaller meals and sacks—try three larger meals and three snacks per day—with foods from all four food groups including produce such as fruits and vegetables, whole wheat products, low fat milk products, and protein such as meat, fish, and eggs.
Take Insulin.
Talk with your physician about insulin injections to manage your blood glucose levels.
Can I get pregnant if I have Type 1 or Type 2 diabetes?
Yes, but it is important to manage your glucose levels, especially during the first 5-11 weeks of pregnancy. This is when the baby’s organs are beginning to develop and if blood sugar levels are irregular, the formation of the baby’s spinal cord and heart could be affected.
LET'S WORK TOGETHER TO FIND A CURE.
VISIT US
1-020 Li Ka Shing Centre
University of Alberta
Edmonton, AB, T6G 2E1
Office Hours
Monday-Friday 8:30-4:00
If you would like to set up an appointment at our office, please set up an appointment by contacting us at
info@abdiabetes.com