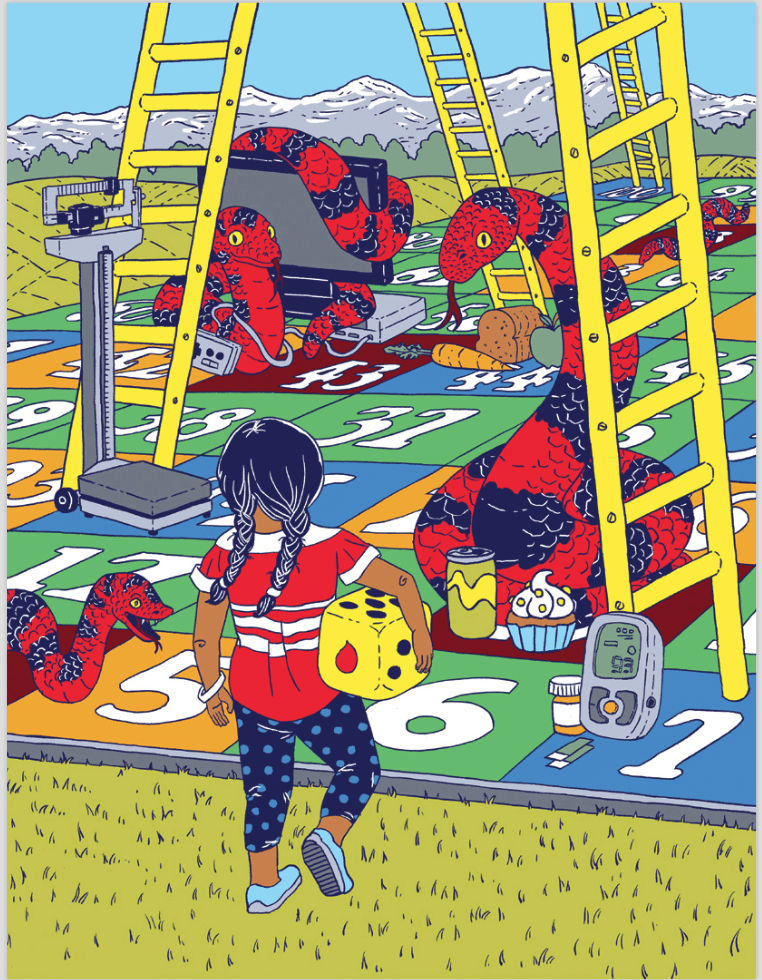
Risky Business
Article by Caitlin Crawshaw. Illustrations by Julia Minamata.
The prevalence of both Type 1 and 2 diabetes is increasing in Alberta. Here’s what you need to know about the risks facing children, pre- and post-diagnosis.
At the Stollery Children's Hospital at the University of Alberta, paediatric endocrinologist Dr. Andrea Haqq diagnoses and treats many of these children. "We're a very busy clinic as we'e been seeing more cases of both Type 1 and 2 diabetes over time," she says. Children with either form of diabetes exhibit many of the same symptoms, including weight loss, frequent urination, and excessive thirst. Occasionally, parents report that their kids are suddenly wetting the bed at night after being potty trained.
Doctors don't know for sure which children will develop diabetes or why. However, a number of risk factors are associated with both forms of the disease and can help predict which kids are more likely to get sick. In some cases, doctors and parents can take action to decrease a child's risk.
Type 1 Diabetes
Environment
Children with Type 1 diabetes require frequent injections of insulin as their bodies don't produce enough of the hormone to process glucose (simple sugar) from food.
It's an autoimmune disease, so immune cells in the body that normally fight harmful things, like bacteria and viruses, mistakenly destroy insulin-producing cells in the pancreas," says Haqq. Unfortunately, the origins of the disease continue to mystify researchers. "We know genetics may play a role in the process, and certain environmental factors like viruses may trigger the disease, but little is known about the exact causes."
Although family history is considered a risk factor, it increases a persons's risk of developing the disease only slightly. Geography is another risk factor as certain communities have higher numbers of people with Type 1 diabetes (including Edmonton), but researchers don't yet know why certain environments create increased risks.
Haqq explains that most people with Type 1 diabetes are diagnosed as children, with the majority diagnosed between the ages of four to seven, and 10 and 14. "These are certain peaks to the disease," she says. Researchers don't know why this is, but speculate that it may have something to do with childhood and diseases and hormones associated with puberty.
With so little known about the causes of Type 1 diabetes, doctors can't offer parents or caregivers any strategies for avoiding its onset. "When we see new children with Type 1 diabetes, it's always important to understand that they didn't do anything to bring on the disease," says Haqq.

Risk Factors for Type 2 Diabetes
Genetics
Unlike Type 1, there's a very strong genetic component to Type 2 diabetes. Having another close relative with the disease or a mother who had gestational diabetes during pregnancy seem to raise a child's risk of becoming diabetic. A child's ancestry can also make him or her susceptible, as Type 2 diabetes tends to be more prevalent among certain ethnic groups (including people of First Nations and South Asian descent). There are also a number of rare genetic disorders that predispose children to obesity such as Prader-Willi syndrome (PWS) (Haqq's research on the disease is internationally known).
Obesity and Unhealthy Eating
Doctors know a little more about Type 2 diabetes, in which the body makes insulin but its cells can't use the hormone properly to break down glucose. Risk factors include poor eating habits and a sedentary lifestyle, but the biggest risk factor is childhood obesity, which has been greatly increasing in Alberta and throughout much of the world. Where a person gains weight raises his or her risk: "Certain fat distributions seem to be particularly bad, like fat in the abdominal region," says Haqq. But genes aren't destiny. Haqq explains that even children with prediabetes who show signs of insulin resistance without having full-fledged diabetes can sometimes avoid the disease with lifestyle changes. Healthy eating, regular activity, and maintaining a healthy weight can mitigate genetic risks of developing Type 2 diabetes. For children who are already overweight or obese, Haqq suggest weight maintenance, not weight loss. She also notes that Body Mass Index (BMI) isn't an absolute measure of health, as a growing body of research show that active people in a higher BMI range can be healthy, too.

Risk After Diagnosis
Whether children are diagnosed with Type 1 or 2 diabetes, they are at an increased risk of a host of health issues over time. Haqq explains that people with diabetes are prone to heart disease, cardiovascular problems, high blood pressure and damage to their nerves, kidneys and eyes.
Mainting optimal blood sugar levels is critical to avoiding these medical complications over time. "We work hard to help people control their levels well in childhood because they have many decades of living with the disease ahead of them," Dr. Haqq says. At the same time, doctors need to be careful not to lower blood sugar levels too much as this can impede a child's cognitive development (growing brains need a certain amount of glucose to thrive).
Children with Type 2 diabetes may also face complications related to obesity including cancer, sleep apnea, stroke, gallstones, osteoarthritis, and infertility. "Obesity is a chronic disease, no different from hypertension," Haqq says. Even when people manage to lose large amounts of weight, our complex biology as human beings make us prone to regaining the weight over time. "People generally have to do something to maintain their body weight," says Haqq. "Obesity requires a lifelong treatment."
LET'S WORK TOGETHER TO FIND A CURE.
VISIT US
1-020 Li Ka Shing Centre
University of Alberta
Edmonton, AB, T6G 2E1
Office Hours
Monday-Friday 8:30-4:00
If you would like to set up an appointment at our office, please set up an appointment by contacting us at
info@abdiabetes.com