Changing Face of Technology in the World of Diabetes
#diabeteseducation
EDMONTON, AB - For a person diagnosed with diabetes, two of the many important tools are an insulin pump and a glucose monitor .
Insulin Pumps
An insulin pump is a small battery-operated device that mimics a human pancreas, which reduces the needs of multiple insulin needle poking throughout the day. In other words, pumps are used to deliver a continuous amount of fast-acting insulin on a 24 hour clock. It is an alternative to daily injections of insulin. The pump can be worn on the body in many places. Normally, it is connected to a narrow plastic tube which is inserted under the skin and taped in place on the patient’s body.
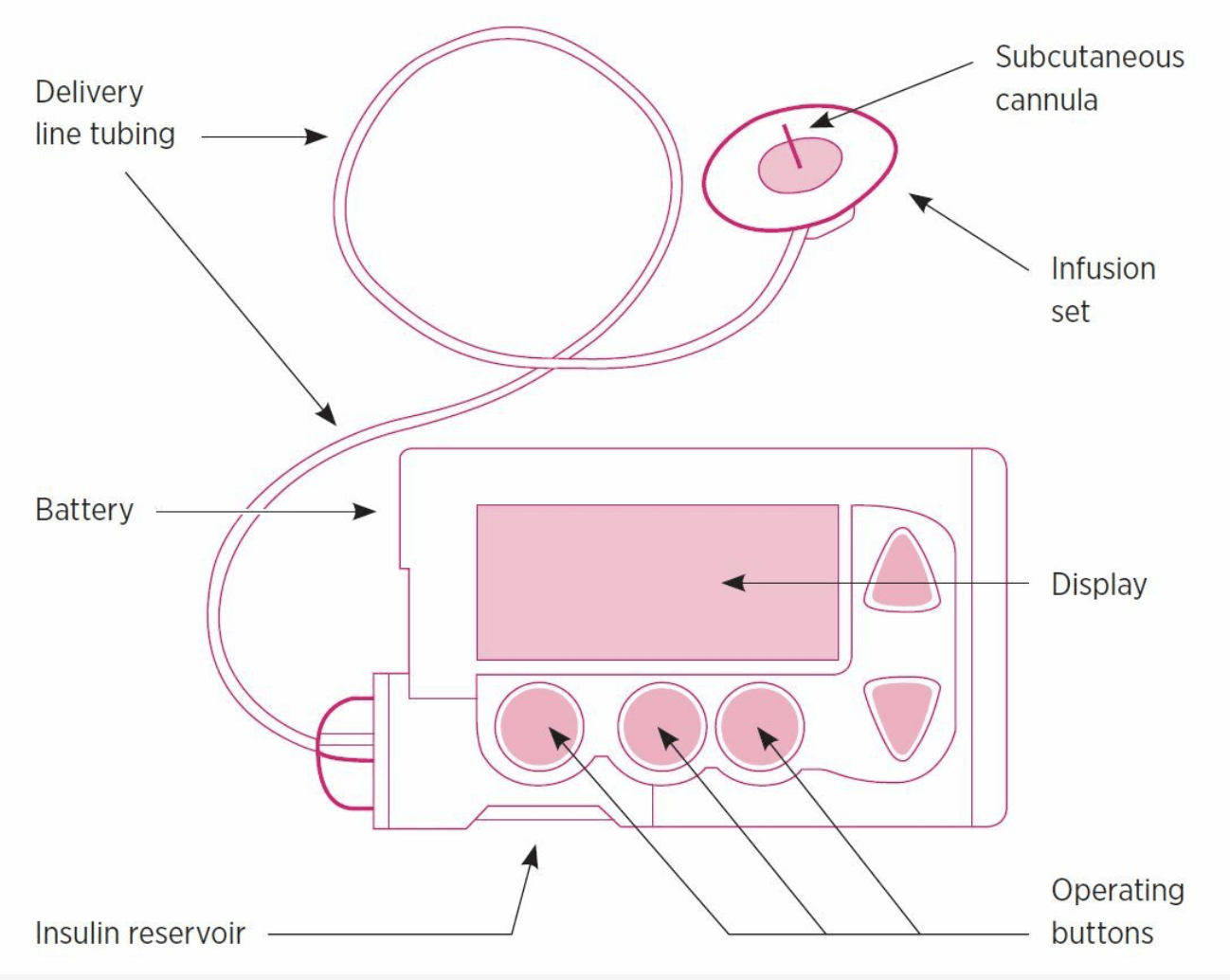
There are three main components to insulin pump therapy:
1. A pump (controlled by a battery) is responsible for pumping insulin in the body.
2. A reservoir holds the insulin.
3. An infusion set contains a thin tube, which runs from the reservoir in the pump to the site of infusion. A short cannula (small tube) is inserted under the skin to get it working.
The cannula is inserted under the skin and held in place by a sticky patch, which can last up to 72 hours. The cannula is connected to the reservoir of the pump that is responsible for transporting a specific amount of insulin to the body.
An insulin pump is programmed with two settings; basal and bolus rate. Basal rate refers to the minimum amount of insulin that is required to maintain a healthy blood sugar level in the body. Whereas, bolus rate refers to the amount of insulin that gets released into the body after a meal is eaten. These settings could be programmed within the insulin pump upon proper instructions and examinations from the patient’s doctor.
The government of Alberta has the Insulin Pump Therapy Program (IPTP) to subsidize a patient in need, who is suffering from diabetes. For a patient to be able to qualify for IPTP, they need to meet two eligibility criteria outlined by the government as well as the clinical criteria developed by the Alberta Health Services (AHS) as mentioned in the IPTP - Clinical Criteria. The Diabetes Insulin Pump Therapy patient resources can be found on here.
Here are a few of the basic eligibility criteria guidelines for an individual to be enrolled as an IPTP participant:
- Be a resident of Alberta covered under the Alberta Health Care Insurance Plan
- Be diagnosed with Type 1 or Type 3c diabetes and under the care of a physician or nurse practitioner.
- Complete a pre-insulin pump information session and an insulin pump therapy education plan.
- Complete a Patient Responsibility Form.
- Meet and continue to meet the clinical criteria as set out in Insulin Pump Therapy Program - Clinical Criteria. The IPTP Clinical Criteria 2019 can be found on right here
NOTE - The diabetes Insulin Pump Therapy patient resources can be found at this link.
If you are looking to apply to be considered for the IPTP program, please visit this link to fill out a self-assessment questionnaire and submit it to your IPTP clinic.
Continuous Glucose Monitoring (CGM)
Continuous Glucose Monitoring (CGM) is the newest way to actively monitor blood glucose levels on a 24/7 clock with minimum efforts required from the patient. CGM is a small wearable device that presents alerts to a patient based on the “real-time data,” which allows the user to proactively manage glucose highs and lows. It also helps the user “gain valuable insights into the impact of meals, exercise, and illness on glucose levels” ( Cofal, 2019 ).
Components of a CGM include a sensor, transmitter, and display device. A sensor is inserted beneath the skin with an applicator, which is held in place by an adhesive patch. The transmitter is a reusable device connected to the sensor that is responsible for delivering real-time-readings wirelessly to the receiver. That information is then visible to the reader through the receiver.

According to Dexcom, the benefits of using CGM are listed below:
- A1C reduction: A1C stands for glycated hemoglobin, a protein that is on the red blood cells which is coated with sugar. Patients diagnosed with Type 1 and Type 2 diabetes are able to decrease their A1C by 1.3%.
- Reduced Hypoglycemia: Hypoglycemia results from low blood sugar levels that can be decreased upon usage of the CGM. It keeps track and alerts you based on real-time depending on other activities that your body has been engaging in.
- Active monitoring at night: CGM provides alerts that warn a patient before a patient approaches lows to highs.
- The biggest benefit of using a Dexcom CGM is that it is reliable. It is designed in a manner that assured alarms go off in the case of hypoglycaemia, which proves to be extremely beneficial during night time for parents who have children with diabetes.
If you are two years of age or older, experiencing frequent hypoglycemia/hyperglycemia, excessive unawareness, going through intensive insulin therapy or other similar experiences could be considered for real-time CGM. Compared to regular glucose monitors, CGM allows the patient to proactively manage diabetes.
Similar to CGM, Freestyle Libre Flash Glucose Monitoring System is convenient, easy, discreet, and user-friendly. The Freestyle Libre sensor is a 35mm to 5mm small device that automatically measures and continuously stores glucose readings day and night. It is meant to be water-resistant that requires no finger prick calibration and could be worn while swimming, bathing or exercising. The sensor is able to scan a person’s current glucose reading, along with last eight hours of glucose data and an arrow showing the direction your glucose is heading. For more details about Freestyle Libre Flash Glucose Monitoring System, visit this link.
Sources
Cofa1. (2019, September 10). What is CGM. Retrieved from
LET'S WORK TOGETHER TO FIND A CURE.
VISIT US
1-020 Li Ka Shing Centre
University of Alberta
Edmonton, AB, T6G 2E1
Office Hours
Monday-Friday 8:30-4:00
If you would like to set up an appointment at our office, please set up an appointment by contacting us at
info@abdiabetes.com